Jan 25
Beat by Beat, Certified Anesthesiologist Assistants Are There for Patients
If you put a child and an older-adult patient in an operating room, how might each react differently to anesthesia?
Nathaniel Flath, CAA, learned about these nuances and many more in his 10 years working as a Certified Anesthesiologist Assistant (CAA).

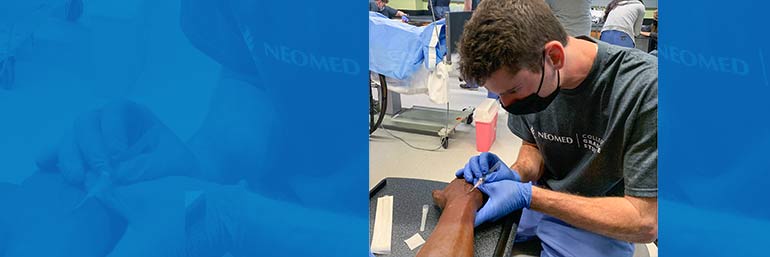
Diverse task trainers such as these mannequin arms give students Easton Black practice with starting intravenous lines on people of various ages, genders and races.
As the program director for NEOMED’s Master of Medical Science in Anesthesia (M.M.Sc.-A.) program, which launched in January, Flath is passing along his knowledge. He understands that CAAs play a critical supporting role in ensuring safe, compassionate patient care.
“That’s why we’re there, beat by beat, by the head of the bed,” says Flath, who also serves as the president of the Ohio Academy of Anesthesiologist Assistants.
Right hand to the physician anesthesiologist
Serving as a much-needed extension of a physician anesthesiologist, CAAs (sometimes more than one) are involved before, during and after surgical procedures. Knowledge and practice, guided by a foundation in compassionate patient care, are key to building the skills needed. That’s why so much of the training in the 28-month M.M.Sc.-A. program offered through the College of Graduate Studies is hands-on in NEOMED’s Research and Graduate Education building, Flath explains.
Health care experience varies among the students in the first cohort. Some have none, while one student has seven years’ experience as a lead respiratory therapist. A phlebotomist, patient care assistants (including one lead PCA who served on hospital committees) and pharmacy techs round out the group.
Whatever their past training or experience, the master’s degree program is designed to prepare them for the in-demand career of a CAA.
Simulation lab training
Standing in front of a mannequin in a simulation lab set up specifically for the anesthesiologist assistant program, Flath points out the three cameras, each from a different angle, that are used to capture each student as they complete mock procedures. Not only is a faculty member watching behind a one-way mirror to provide students with feedback. Videos and comments are also provided to each student afterward for study and review.

Students learn on both humans and mannequins (task trainers). Amanda Narducci (seated), an assistant professor in the College of Graduate Studies, allows student Patrick Varley to start her IV.
Because of the multiple camera angles, students can see what they looked like to the (simulated) patient as well as to their colleagues. It is important not only to remain composed at all times, but also to appear composed at all times, says Flath.
“The student might think, ‘Well, I know what I look like,’ but others may see things that you’re not aware of. We talk a lot to students about controlling your facial expressions.”
The CAA: Providing a human connection
Actually, the need for self-awareness begins before setting foot in the OR.
The CAA’s job begins when they meet a patient in the pre-operative care unit, equipped with data provided from the patient’s chart that has been discussed with the attending anesthesiologist. Putting the patient and family at ease is important for the patient pre-procedurally and helps provide a safe, smooth transition for the start of anesthesia and the procedure.
“Patients also feel reassured when we remind them that we will stay with them throughout their procedure,” says Flath.
You can’t overestimate the importance of the human connection provided by a CAA, he says. For example, Flath recalls a time when he was working as a CAA and the patient was a terrified girl in her teens who was having a tumor removed.
“There must have been 15 members of her family in the room. She was crying and when she saw that her family was upset, too, it made her more upset. So, I sat down next to her and asked her questions — where does she go to school and what does she like to do for fun? I was able to get her to laugh. And that’s one example of why I find this career so rewarding: Because I could take someone from tears to laughter at one of the scariest times of her life.”
During a procedure, the CAA and the attending anesthesiologist carefully guide the patient to a comfortable sleep state in preparation for the procedure. The CAA will stay by the patient’s side throughout the procedure, closely watching the monitors and making any adjustments needed for the patient or the procedure. They don’t only watch; they listen, too. The pitches and the pacing of the tones coming from the monitors actually communicate details about the patient’s health and safety.
After the procedure, the CAA wakes the patient and checks to make sure that pain and nausea are well controlled, then gives a report to the nurse in the post-operative care unit who will oversee the patient’s care.
Anesthesia Fun Camp
Although the 12 students in this cohort are training for a highly responsible role, Flath likes to add a light touch to their time at NEOMED, knowing that a more relaxed student will learn more easily. So, while the first four weeks of classroom and sim lab time are intense (“Plan to talk to your loved ones after the four weeks,” Flath tells the students, only half-jokingly) the director has dubbed it Anesthesia Fun Camp.
This foundational first month is a combination of classroom work as well as hands-on simulation in a mock operating room with a state-of-the-art, high-fidelity patient simulator.
The students touch on many different topics so when they study them in depth later, they’ll have a point of reference. During their second week, for example, students spent a morning learning and practicing airway management skills such as intubation, bag-mask ventilation and use of other airway devices. The afternoon was devoted to IV workshops, practicing both with task trainers (mannequins) and on each other.
Two fourth-year College of Medicine students – Anuradha Kanaparthi and Josh Engle – volunteered their time to help at those sessions.
“The beauty of a sim lab is that students can practice a technique or procedure as many times as it takes for them to become comfortable with it – before they ever set foot in an operating room,” says Flath.
Anesthesia clinical rotations
In week five, students will head off to clinical rotations at area hospitals.
It’s going fast and well, says student Mitchell Harshbarger. “Despite the short time I have been on campus, I feel like I have learned a lot. It is hard to believe that only a few weeks ago, I would not have been able to understand what we have been talking about every day,” he said, adding, “I cannot wait to continue learning.”

